The menopause in pictures
The menopause in pictures is a visual guide in six images, giving you a visual overview of this complex time in a woman’s life, along with some of its consequences and treatments.
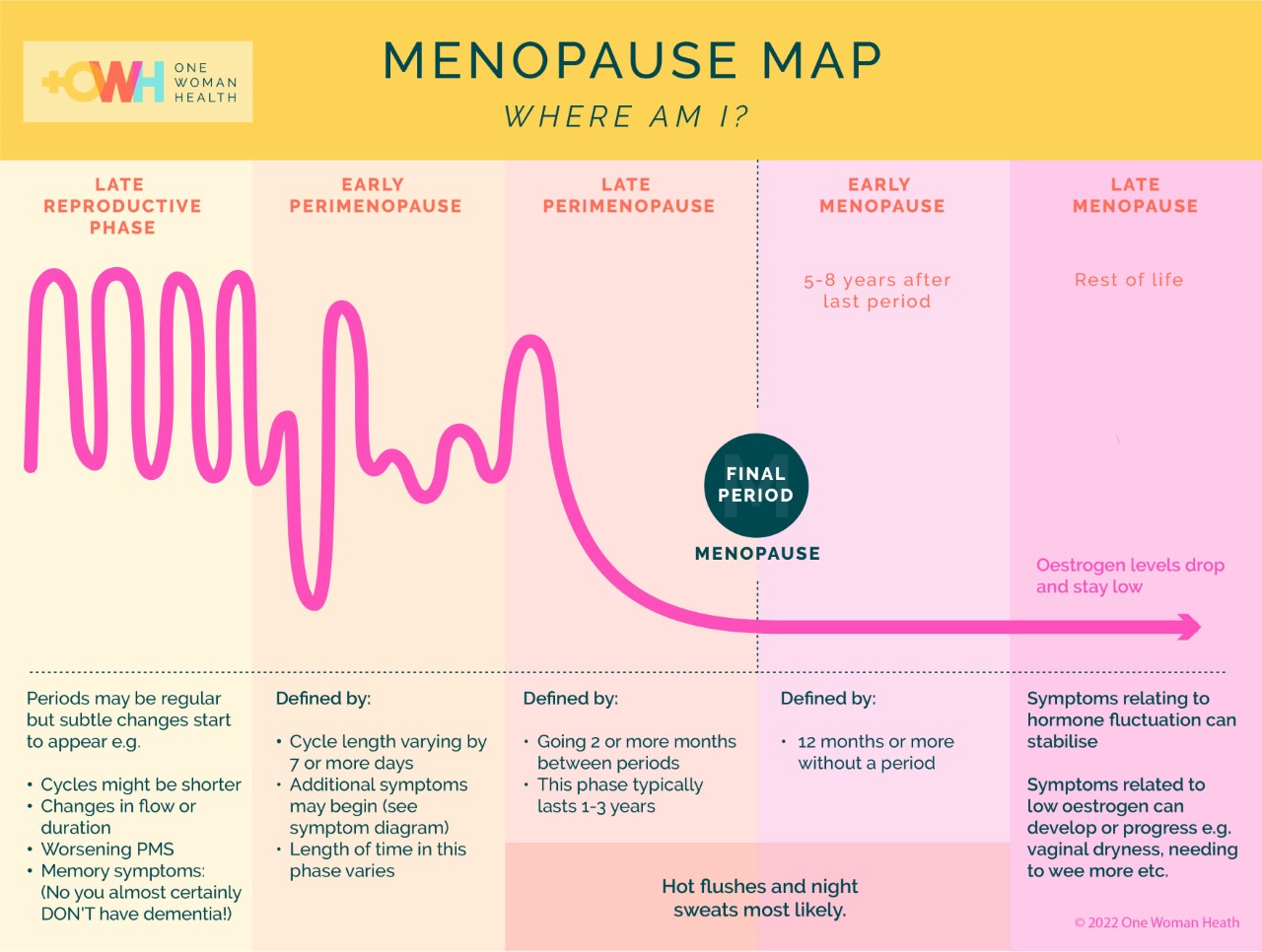
1. A Map for the Menopause
The menopause doesn’t happen overnight. The shift in hormones, periods and potential for symptoms changes over years. While the word ‘menopause’ describes the complete end to periods, the ‘perimenopause’ is the time (often years) before and after where women notice changes and experience symptoms. Women often ask ‘is it menopause?’ and ‘where am I in all this?’ It can be helpful to see an overview of the process to pinpoint where we are now and understand what might be coming up.
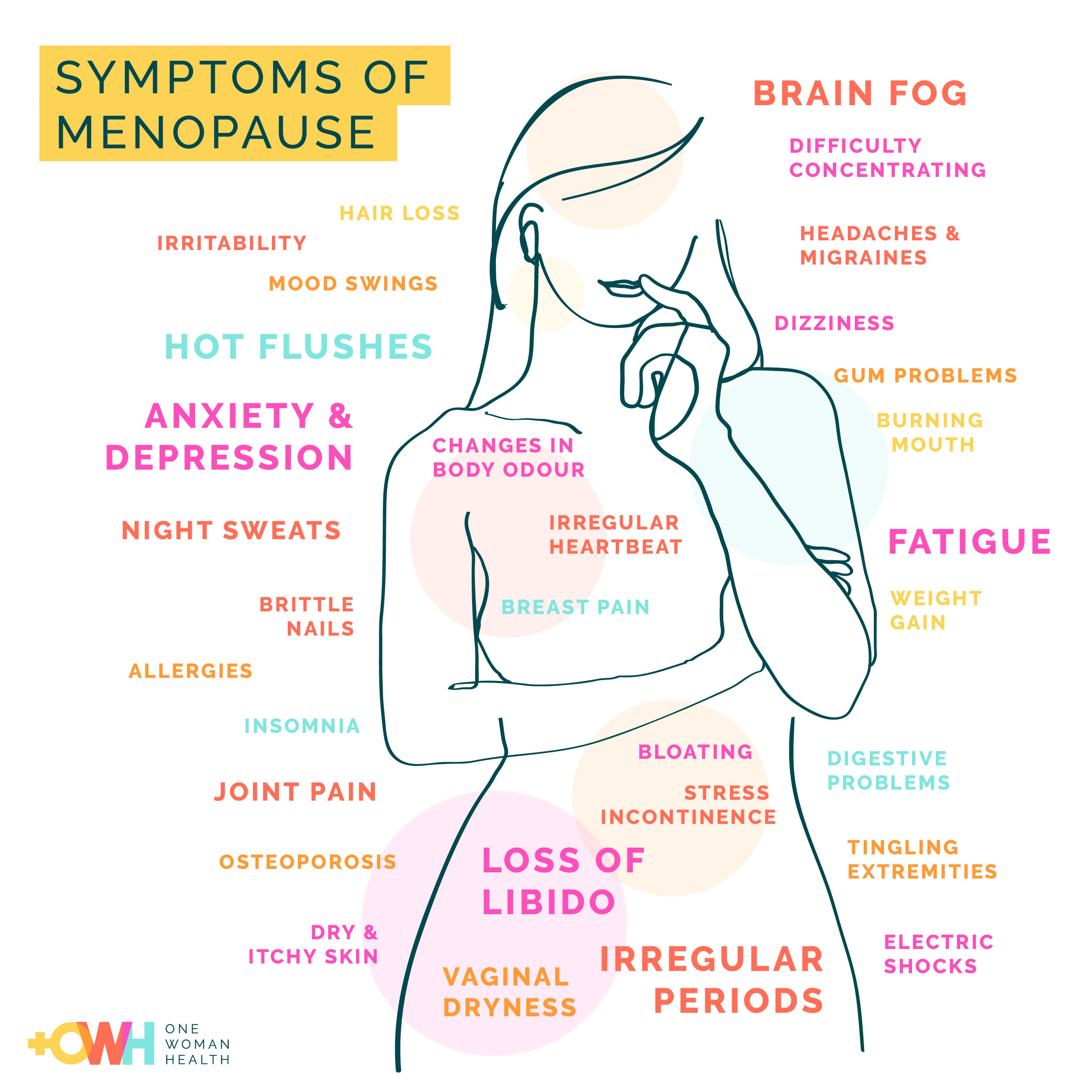
2. The Symptoms of Menopause
With over 34 recognised symptoms of menopause, it can cause more than the stereotypical hot flushes and night sweats. Some of the most problematic symptoms can be mood changes, migraine, disturbed sleep, fatigue, joint pain. In perimenopause, changes in bleeding pattern can wreak havoc on daily life. Later on, vaginal discomfort is a little talked about symptom which women do not need to suffer in silence. Every symptom has at least one other possible cause, so it can be helpful to talk to a specialist who can look at the whole picture with you.
3. Changes to body chemistry
Whether you experience symptoms or not, the drop in female hormones around the time of menopause triggers wider changes to our metabolism that we can’t see. We might notice this as a gain in weight around our middle, or increased desire for sugary food. We almost certainly won’t be aware of the changes taking place to our bone, shown in the diagram below.
We reach peak bone density (strength) in our 30s and after this is, it starts to decline (get thinner and weaker). The speed at which we lose bone increases around the time of the final period (2-5% per year) before levelling off again to a steady loss of 1-2% per year . Some people lose bone faster than others, and there are external factors that influence this too. If you want to keep your bones strong into older age, midlife is the ideal time to take action.
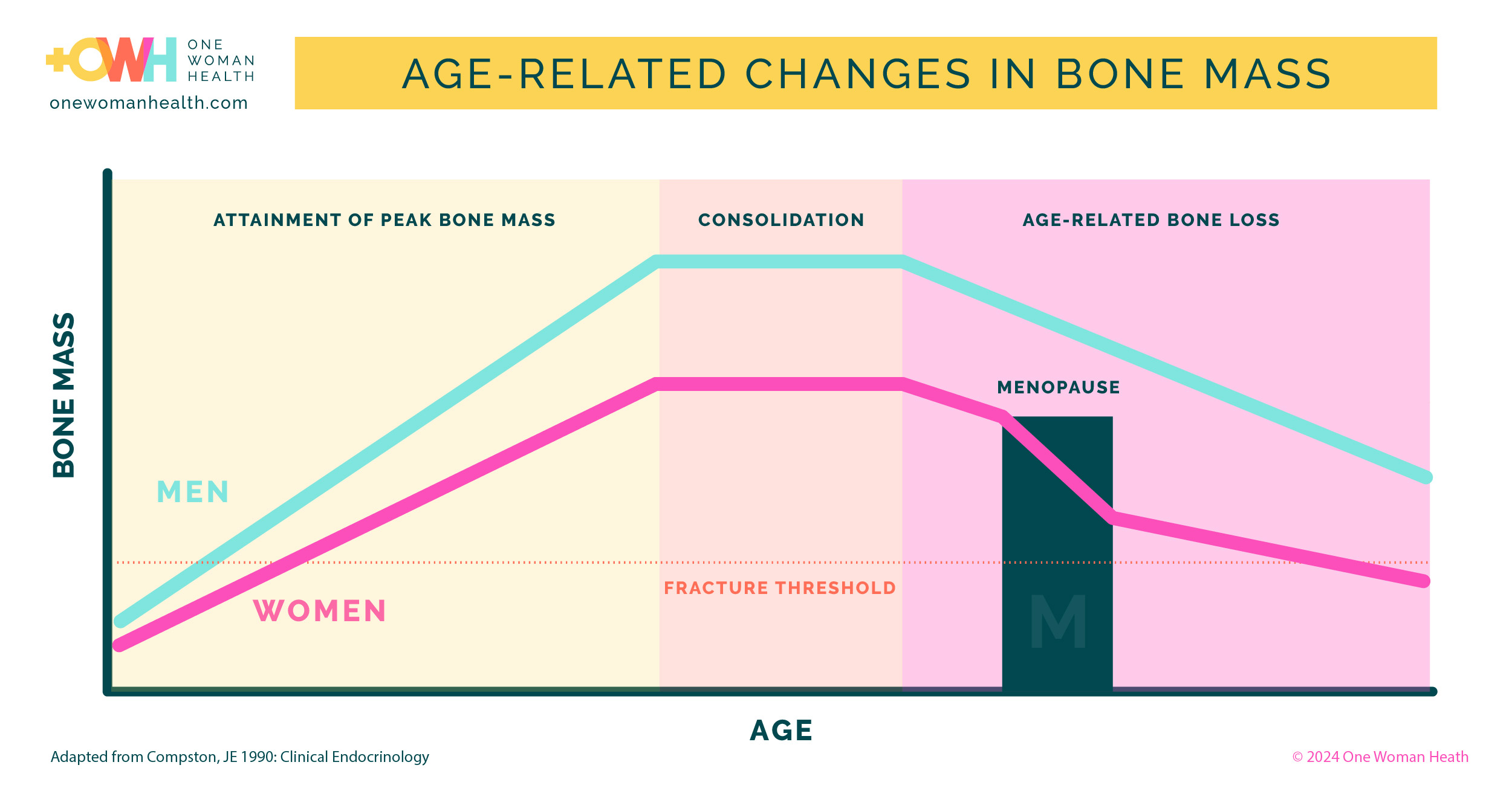
(Compston JE 1990 ;Clinical Endocrinology)
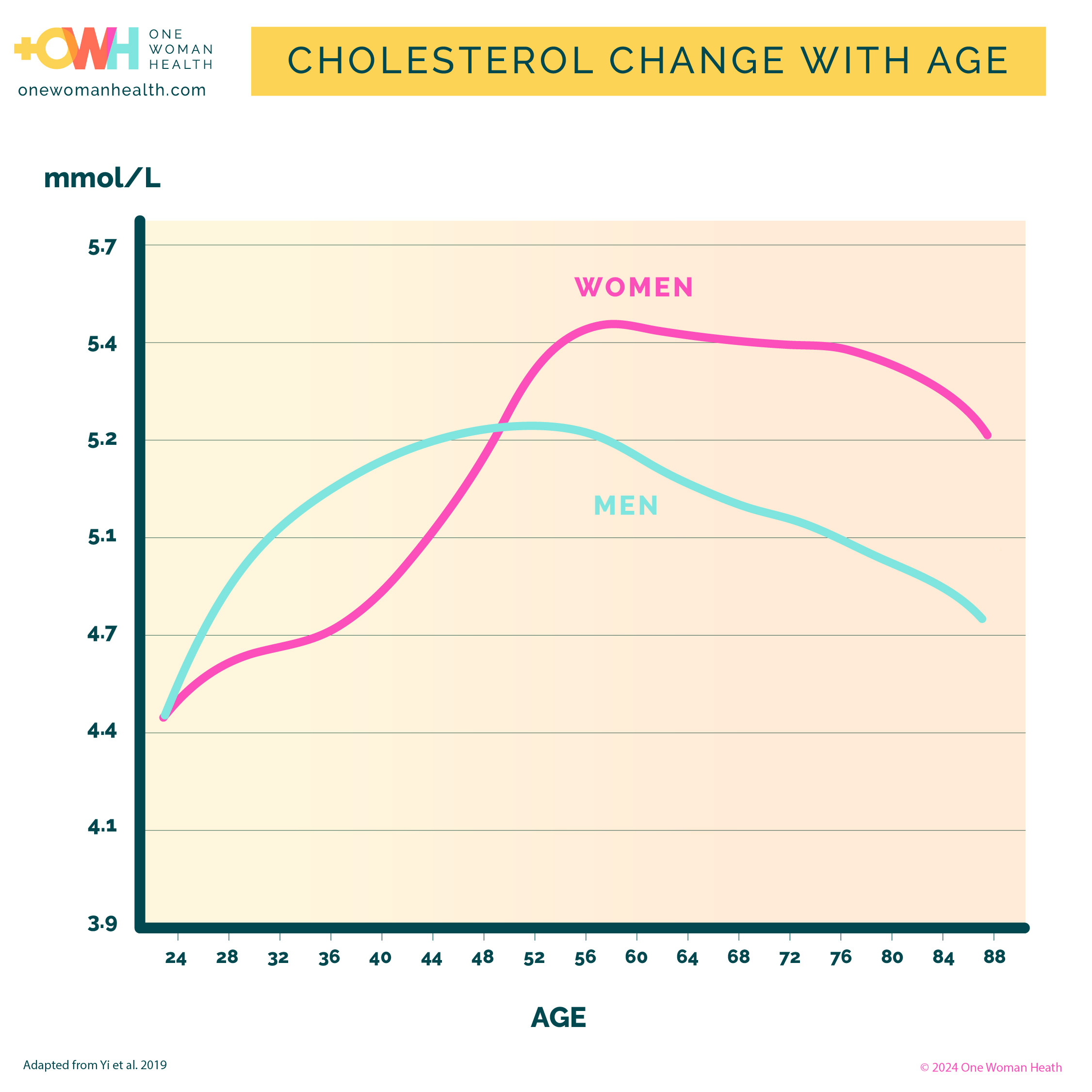
4. Changes to blood cholesterol
We tend to think of cardiovascular disease – diseases caused by the furring up of our arteries and blood vessels – as something that affects more men than women. It includes heart attack, heart disease, stroke, certain kinds of dementia. Although women tend to be affected 7-10 years later than men, overall the absolute numbers are approximately the same.
Until the average age of menopause, women are relatively protected compared with men. However, with age plus the loss of oestrogen, our cholesterol levels can overtake men at this point, increasing our cardiovascular risk. Most women are not aware this is likely to happen, but it’s the ideal time to find out your cholesterol level and wider lipid profile, so you can keep your arteries healthy!
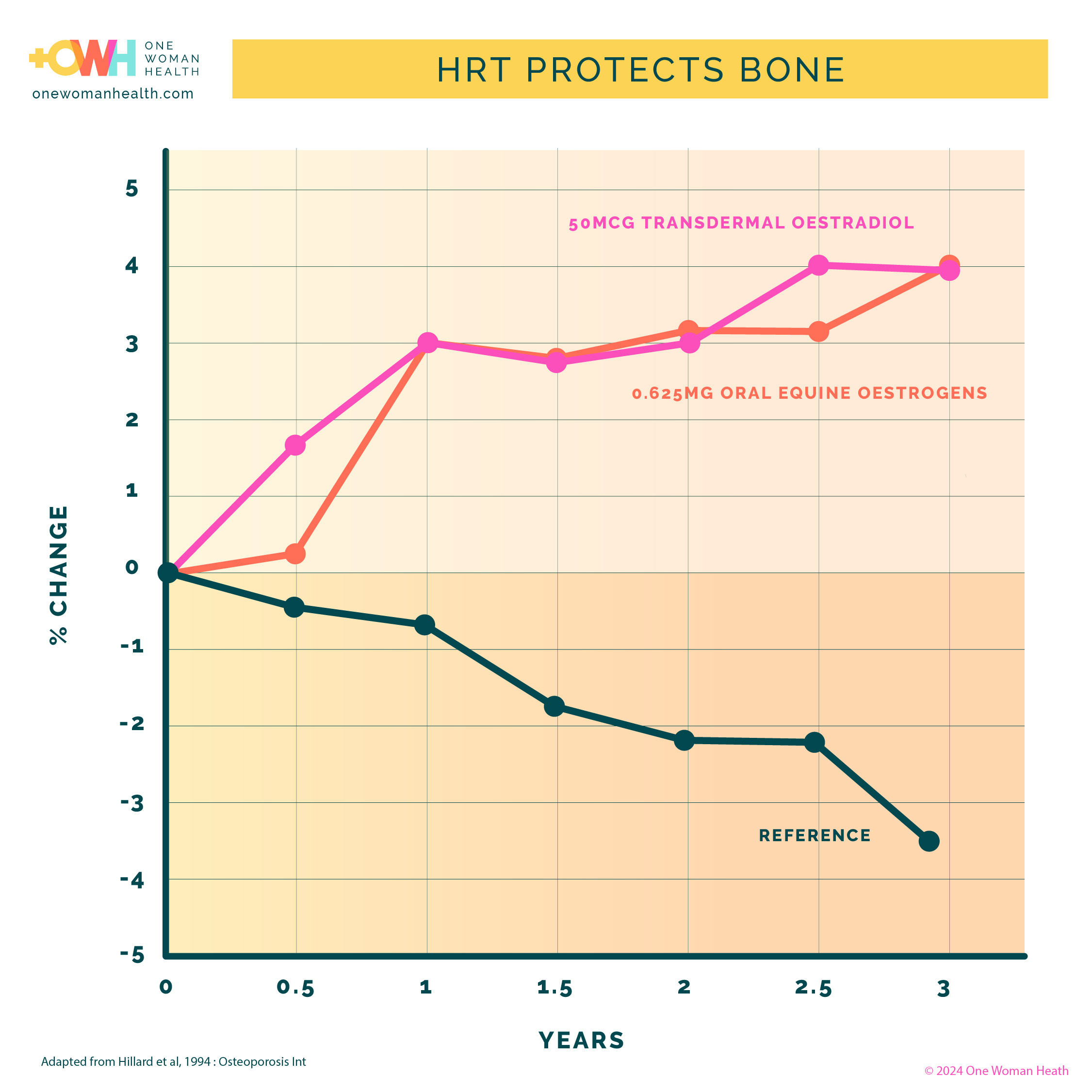
5. The effect of HRT on bone
Replacing oestrogen maintains bone strength. The graph below shows that oestrogen can increase bone density by 3-6% and maintain it over time. The reference line below is ‘no HRT’. As we saw in (3) with very low levels of oestrogen, we gradually lose bone density. Women who take HRT to treat symptoms will also get the benefits of bone protection, while they take HRT, reducing their risk of fracture.
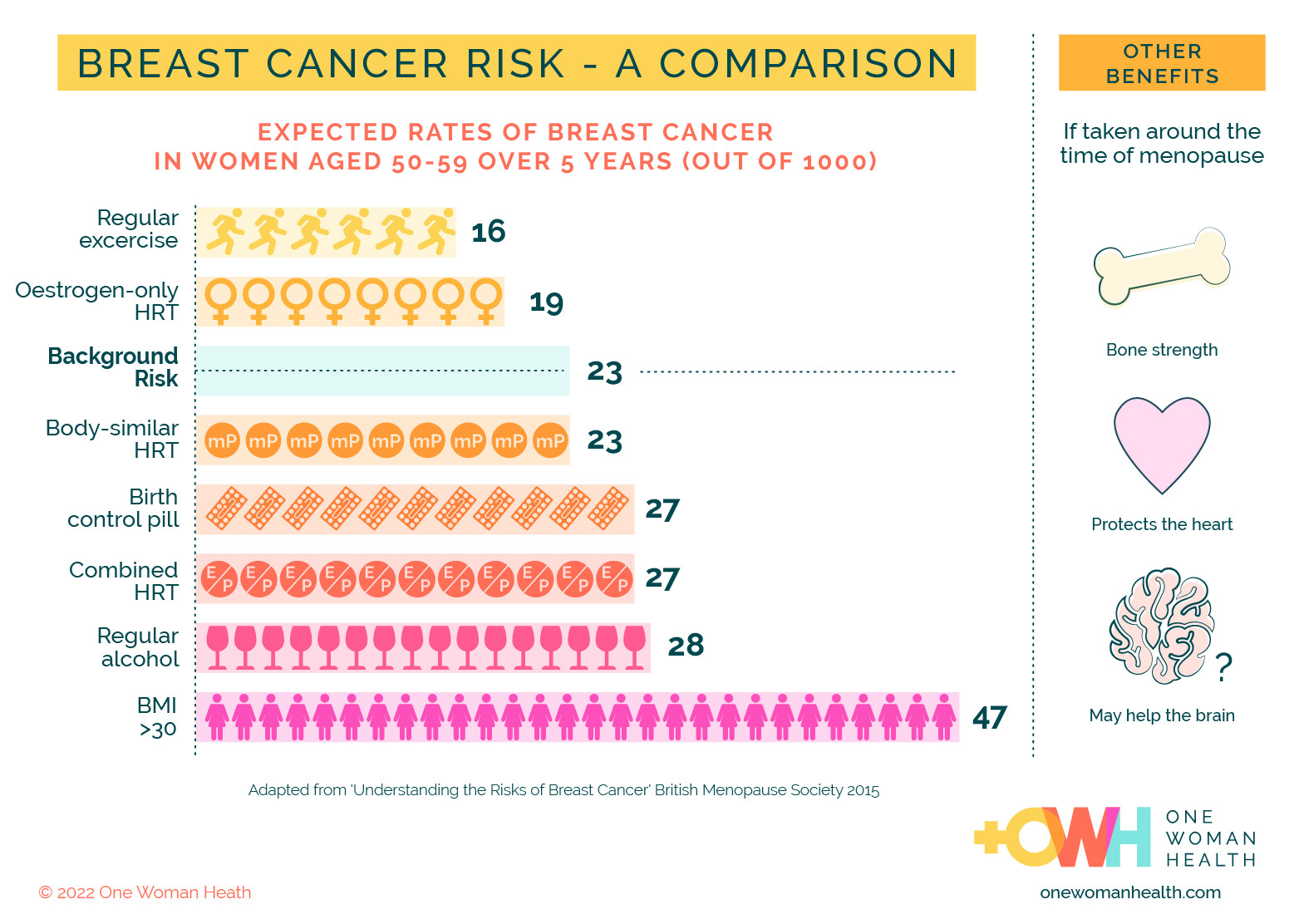
6. Risks of HRT
Many women understandably want to know if there are risks associated with taking HRT. The good news is, that for most women, the benefits, in terms of quality of life and longer term benefits, will outweigh the risks. However, it very much depends on the individual and your doctor can take you through what it means for you.
One important thing to remember is HRT is not one medicine. Exactly what you have and how you take it can minimise any risk. Since the publicity in the early 2000s around HRT and breast cancer, this is a common question. The chart below aims to put this into context.
Breast cancer is a common condition and therefore everyone has a background risk. It can be influenced by things that you can’t do anything about (family genetics) and things that you can (whether you exercise or regularly drink alcohol, for example). Taking hormones, including contraceptives, influences risk. We have some evidence that suggests that if we take hormones that are more similar in structure to the ones we produced in our own body, the risks are lower, and that is reflected here. Research is ongoing.